An Open Letter to a NYTimes Reporter
On convincing traditional media to cover new approaches in pain management
Dear Voyagers,
A couple of weeks back I opened Instagram to see a writer friend of mine sharing a newly published New York Times Magazine article whose title seemed promising:
I couldn’t agree more! “YAY,” I thought to myself. “The word ‘revolution!’ This piece will definitely cover mindbody science.” I raced through the 6,500 word story, scanning lots of information I already knew, excited to learn some things I didn’t know, and even more excited to see mentions of the mindbody work that has helped me so much in the past year. When I finished, assuming I missed the obvious due to my fast read, I sat down again and read the piece again, thoroughly, in detail.
Alas, dear reader, no amount of reading could reveal something that was not there. The piece included not one mention of Dr John Sarno, Dr Howard Schubiner, Nicole Sachs, of Pain Reprocessing Therapy (PRT), Tension Myositis Syndrome, or the Curable app. No discussions of how, in sensitive people (people I call Voyagers1) the medicalization of chronic symptoms can lead to deeper and deeper holes of suffering. Instead, the article did exactly what other articles have done over the years, plunging deeper into the wishful thinking of a medicalized approach to chronic pain.
In other words, the piece decided to opt out of the fascinating new paths that are being forged by innovative thinkers in the space and stay with the tried and true — an approach that seems to be healing very few people. Indeed, the author herself ends the piece, “It’s hard not to wish for a real fix: one in which I’m magically returned to the body that, for years, simply worked.” My heart goes out to her. I know that feeling and desire.
But I couldn’t just sit by and continue to allow this dominant narrative to play out without at least attempting to get more voices into the mix. Since the author is a friend of a friend, I was able to get her email address, and I decided to write her, along with fellow my friend-in-healing Andrea de Oliveira. This is the note we sent along.
Dear Jennifer,
I got your email address from [NAME], a mutual friend. Also on this email: Andrea de Oliveira, a friend / fellow student of chronic pain management who I’ve been partnering with on research into new approaches to pain management.
Briefly, our background: We both work in tech (Andrea was a product manager at Twitter who now works in the tech / behavioral health space at AnswersNow), and I work at Pinterest’s product incubation lab in the innovation space.
We're reaching out after reading your chronic pain article just published two days ago in the New York Times. We appreciated the research and work you put into the piece. Across our shared decades navigating chronic pain, we resonated a lot with the experiences that you shared — the specialist hopping, the gamut of medical exams and the experimental treatment protocols. We have lived these experiences as well and think you did a fantastic job of summarizing a very common pattern in the space. We also appreciated your recap of research citing chronic pain as a CNS2 disorder. We’ve also spent time with that same research.
But we felt you were missing something very important, and that’s why we’re reaching out to you now.
Andrea and I, out of desperation, came across a new and developing line of research and chronic pain treatment focusing on the impact of chronic stress and tension on the nervous system which leads to chronic pain. Although still early, randomized clinical trials have shown that these treatments significantly outperform existing options for chronic musculoskeletal pain, somatic symptom disorder, and chronic back pain.
What we learned about psychophysiological treatments was incredibly eye-opening for both of us. Our learnings were far from theoretical: This new approach led us both to full recoveries from conditions including endometriosis, IBS, Hashimoto’s thyroiditis, chronic fatigue syndrome, chronic migraines, and chronic whiplash with neuropathy. This approach, designed to correct nervous system dysregulation and impact chronic pain symptoms, originated with Dr John Sarno. In the past decade, this type of chronic pain research has expanded exponentially thanks to the work of Dr Howard Shubiner.
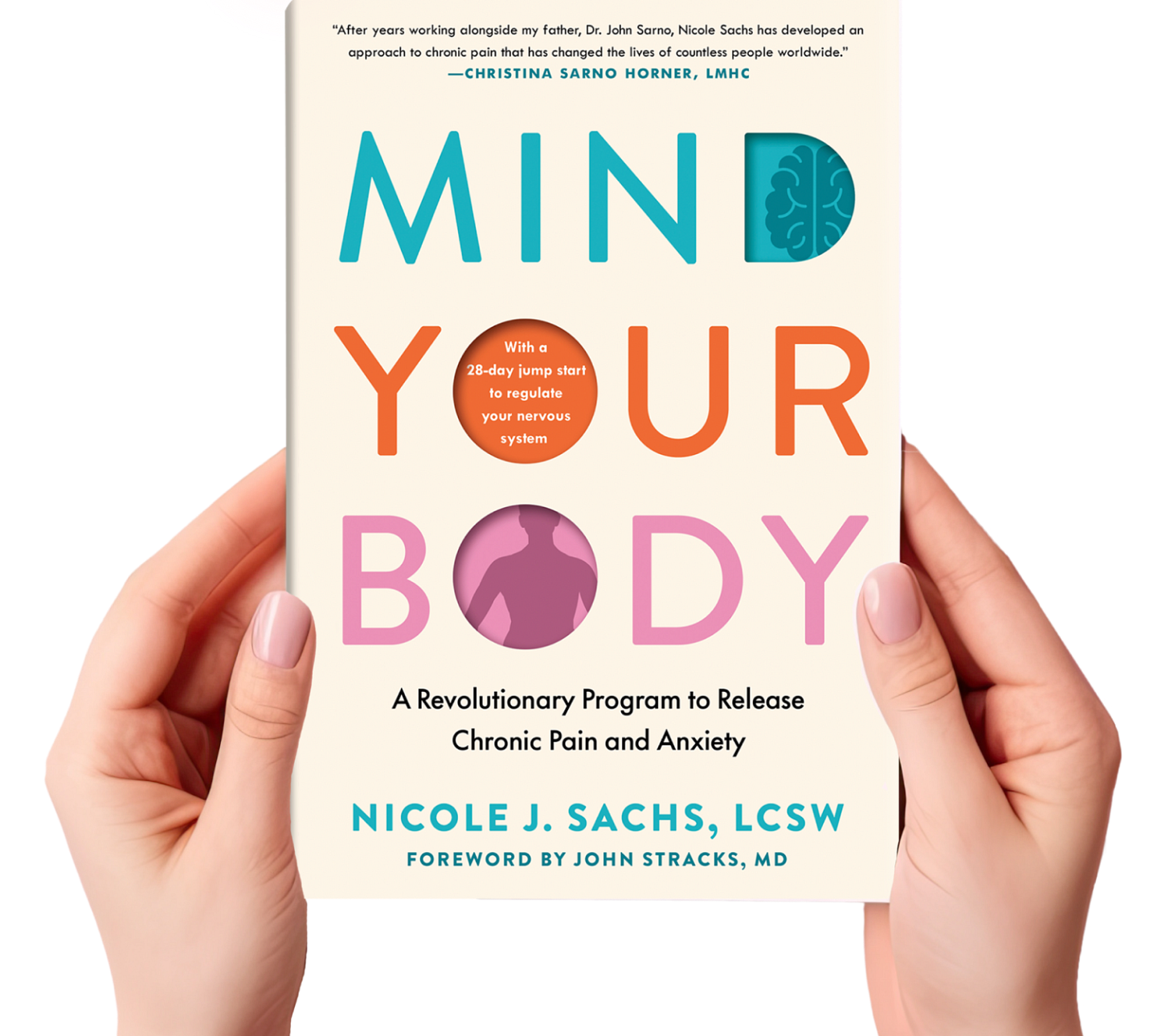
A new book on this topic by Sarno acolyte Nicole Sachs is coming out next month and we hope it will hit your radar if you plan to continue digging into chronic pain. We are spending this time writing to you because we believe that this new line of research is the missing puzzle piece for the billions of people suffering from chronic pain. The innovation part of me wants you to know this exists not just for your reporting, but also for your health.
We would be honored to get to talk to you about this via Google Chat if you have any interest at all – we genuinely think this work could change lives,
Meredith + Andrea
It’s been two weeks and we’ve gotten no response from Jennifer, but that’s okay. The older I get, the more I’ve learned that I cannot expect everyone to jump onboard the same bandwagon at the same pace. My hope is that if I simply share what I’m learning in a straightforward enough way, some of the right people will start to get curious. They will open their minds to the possibility that chronic pain3 is more complex than a broken leg, and will require a much deeper, more nuanced, at-times-counterintuitive approach. And they will listen to the stories of the people who are healing from chronic pain through the hard work of changing their neural pathways in small ways, day by day.
If you are currently experiencing chronic pain and want to know what steps to try next, here are two good places to start:
Whether you are familiar with this work or not, I’d love to hear from you. Are you skeptical of this healing path, or curious, or both? What part of the work interests you — what would you like to hear more about? Let me know.
Voyagers are the people who make up the Beautiful Voyager community. At heart, we’re a bunch of sensitive internal travelers. Yes, Voyagers are overthinkers, people pleasers, and perfectionists, but that’s really shorthand for a certain type of person who struggles with stress, anxiety, and overthinking. Some may describe Voyagers as Highly Sensitive People, others may talk about our easily stimulated brains, and of course the word “neurotic” will be salad dressing tossed into the mix. But however you make sense of these traits, they are special, and they are what make up the Beautiful Voyager community. Explore the Voyager Lighthouse map to read the messages in a bottle shared by other Voyagers around the world.
Central Nervous System. “One of the big insights of the past decade is that chronic pain is a disorder of the central nervous system,” Gereau, Director of the Washington University Pain Center in St. Louis, told me. “It has been a huge change in how we understand these conditions. Before, we were basically just mystified by persistent pain.”
Pain that lasts longer than the normal healing time, or beyond several months.







Well done you for doing your best to spread the word. Can't wait for Sachs' book!!
Thank you SO much for reaching out to the author, and also for mentioning us here! We also read this article with disappointment, not least of which for all the patients reading who received another hit of fear and discouragement from this perspective. Keep up the good fight!
Sarah (from Team Curable)